Foraminal stenosis, also known as foraminal narrowing, is a condition where the neuroforamen becomes constricted. These openings are the passageways for the spinal nerves to exit the spinal column and travel to the rest of the body. When a neuroforamen narrows, it can compress or pinch the nerve root passing through it, leading to pain and other symptoms in the area supplied by that nerve.
Foraminal Stenosis
Overview
Causes
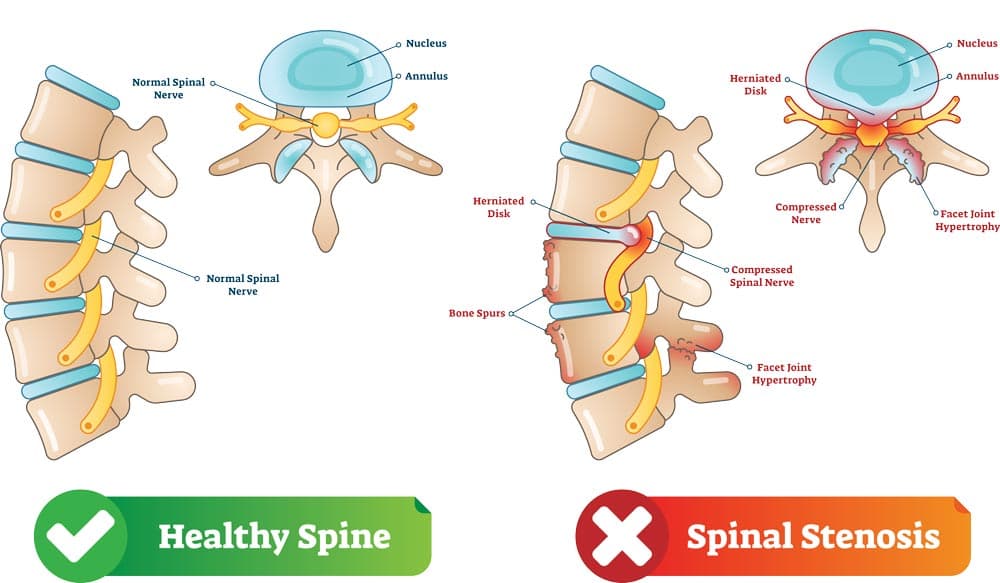
Foraminal stenosis is most often caused by age-related degeneration and wear and tear on the spine. Key contributors include:
- Degenerative Disc Disease: As the discs between your vertebrae dry out and flatten, the space of the neuroforamen shrinks.
- Bone Spurs: The body may grow small, bony projections (osteophytes) to try and stabilize the spine, but these can grow into the foramen and press on the nerve.
- Herniated Discs: A ruptured disc can protrude into the foramen, causing direct compression of the nerve.
- Facet Arthritis: The small joints in the spine can become inflamed and overgrown, which encroaches on the exiting nerve.
Symptoms
The symptoms of foraminal stenosis depend on which part of the spine is affected (cervical, thoracic, or lumbar). Cervical nerves affect the shoulders and arms while thoracic nerve affect the chest and abdomen. The most common region is the lumbar nerves which affects the buttocks and legs.
- Pain: The most frequent symptom, which may be a dull ache or a sharp, shooting pain radiating along the path of the affected nerve (e.g., from the spine to the hand or foot).
- Numbness and Tingling: A "pins and needles" sensation or a loss of feeling in the affected limb.
- Muscle Weakness: In severe cases, the nerve may become so compressed that it causes weakness or loss of coordination in the muscles it controls.
Non-Surgical Treatments
- Physical Therapy and Exercise: Strengthening core and back muscles to improve stability, as well as nerve gliding stretches, can alleviate the pressure on the nerve.
- Lifestyle modifications: Maintaining a healthy weight and avoiding activities that aggravate the pain.
- Medications: Over-the-counter anti-inflammatory drugs (ibuprofen, naproxen) are preferred first-line medications. Stronger prescription medications may be considered if these fail, including nerve pain medications or short-duration oral steroids.
- Injections: Occasionally, steroid injections can provide temporary relief by reducing inflammation around the foramen and nerves.
Surgical Treatment
Surgery is considered as a last resort when non-surgical options have failed and the patient is experiencing severe, debilitating pain or concerning neurologic deficits.